« PS:Dissection aortique (diagnostic) » : différence entre les versions
De wikiDMU2
(Page créée avec « == Evaluation du risque == upright == Algorithme D-Dimères == upright == Référence == link=&nb... ») |
m (→Cible :) |
||
| (4 versions intermédiaires par 2 utilisateurs non affichées) | |||
| Ligne 1 : | Ligne 1 : | ||
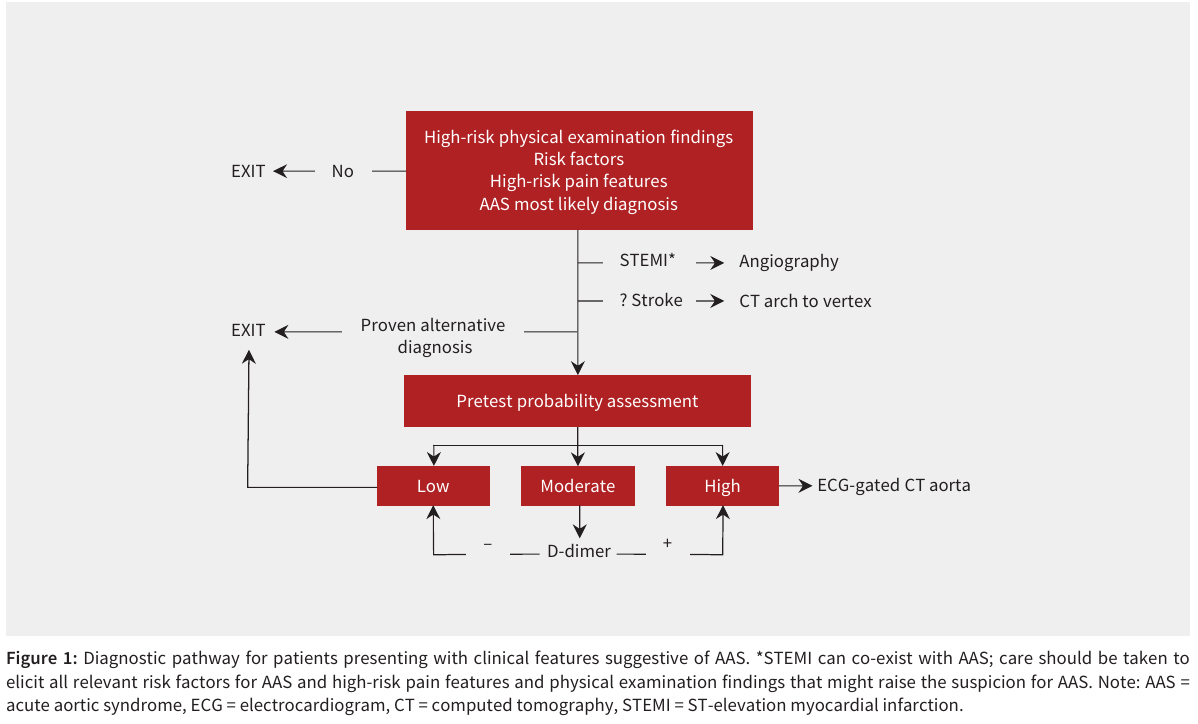
== Algorithme == | |||
[[File:DAo ddimeres.png|upright|DAo ddimeres.png]] | |||
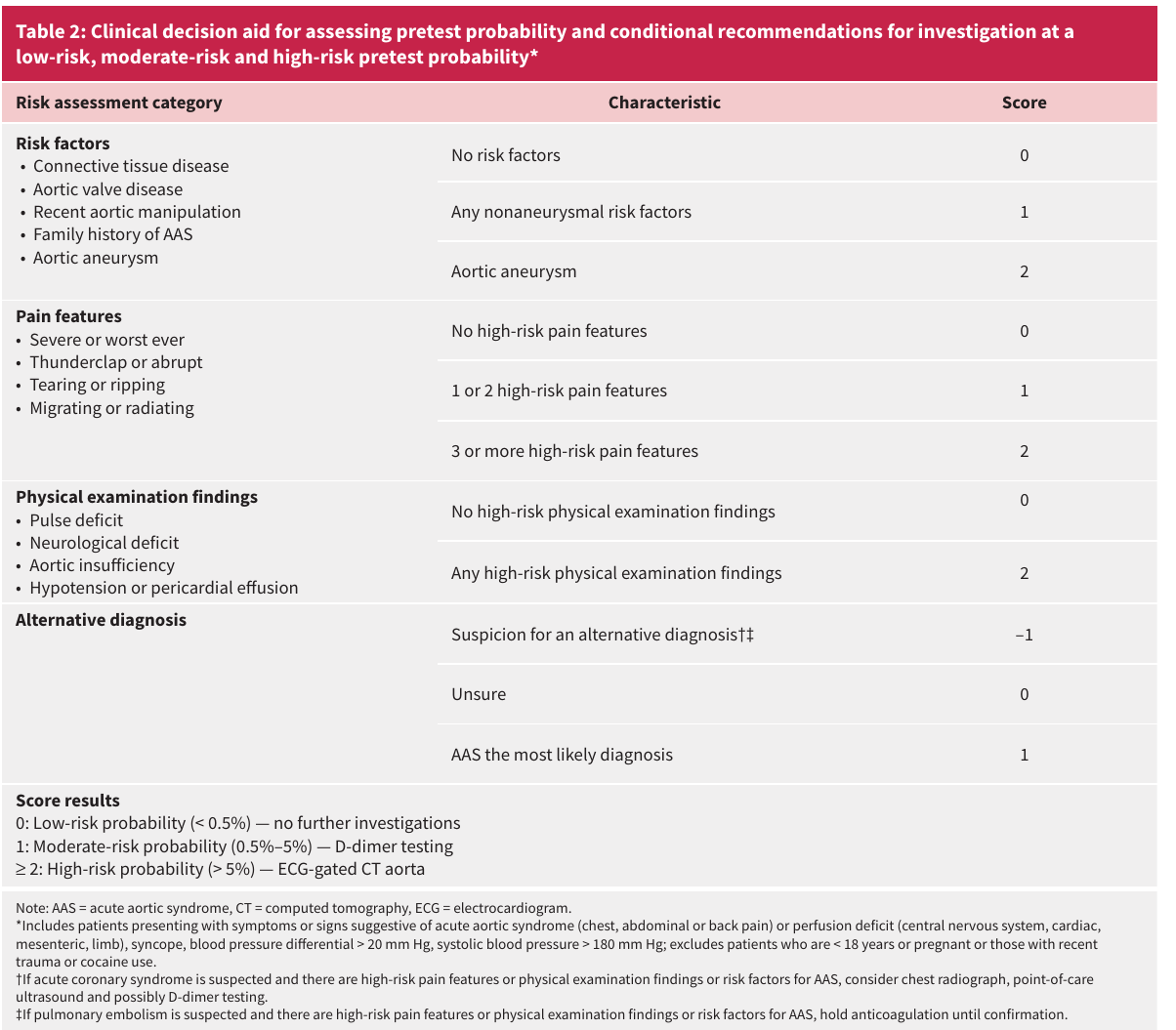
== Evaluation du risque == | == Evaluation du risque == | ||
[[File:DAo risque.png|upright]] | [[File:DAo risque.png|upright|DAo risque.png]] | ||
== SPEED protocol == | |||
Utilisation de l'ECMU : Le protocole SPEED combine l'échocardiographie transthoracique et l'échographie de l'aorte abdominale. | |||
=== Cible : === | |||
*dissection aortique de type A de Standford | |||
***épanchement péricardique, | |||
***un flap intimal | |||
***un diamètre de l'aorte initial (AOFT) > 35 mm mesuré d'une paroi interne à l'autre à 20 mm de l'anneau aortique en fin de diastole<br> | |||
*dissection aortique de type B de Standford | |||
***un flap intimal dans l'aorte abdominale | |||
=== valeur du test === | |||
{| class="table article-section__table"<thead> | |||
|- | |||
| class="bottom-bordered-cell right-bordered-cell left-aligned" style="width: 80px;" | | |||
! class="bottom-bordered-cell left-aligned" style="width: 213px;" | A-AoD and B-AoD (95% CI) | |||
! class="bottom-bordered-cell left-aligned" style="width: 126px;" | A-AoD (95% CI) | |||
! class="bottom-bordered-cell left-aligned" style="width: 276px;" | B-AoD (intimal flap only) (95% CI)</thead> | |||
|- | |||
| class="right-bordered-cell left-aligned" style="width: 80px;" | Accuracy | |||
| class="left-aligned" style="width: 213px;" | 91 (89.3–92.5) | |||
| class="left-aligned" style="width: 126px;" | 91.1 (89.4–92.6) | |||
| class="left-aligned" style="width: 276px;" | 99.8 (99.3–100) | |||
|- | |||
| class="right-bordered-cell left-aligned" style="width: 80px;" | Sensitivity | |||
| class="left-aligned" style="width: 213px;" | 93.2 (81.3–98.6) | |||
| class="left-aligned" style="width: 126px;" | 100 (83.9–100) | |||
| class="left-aligned" style="width: 276px;" | 87 (66.4–97.2) | |||
|- | |||
| class="right-bordered-cell left-aligned" style="width: 80px;" | Specificity | |||
| class="left-aligned" style="width: 213px;" | 90.9 (89.2–92.5) | |||
| class="left-aligned" style="width: 126px;" | 90.9 (89.2–92.5) | |||
| class="left-aligned" style="width: 276px;" | 100 (99.7–100) | |||
|- | |||
| class="right-bordered-cell left-aligned" style="width: 80px;" | PPV | |||
| class="left-aligned" style="width: 213px;" | 26.3 (19.6–33.9) | |||
| class="left-aligned" style="width: 126px;" | 15.4 (9.8–22.6) | |||
| class="left-aligned" style="width: 276px;" | 100 (83.2–100) | |||
|- | |||
| class="right-bordered-cell left-aligned" style="width: 80px;" | NPV | |||
| class="left-aligned" style="width: 213px;" | 99.7 (99.2–100) | |||
| class="left-aligned" style="width: 126px;" | 100 (99.7–100) | |||
| class="left-aligned" style="width: 276px;" | 99.8 (99.3–100) | |||
|- | |||
| class="right-bordered-cell left-aligned" style="width: 80px;" | '''PLR''' | |||
| class="left-aligned" style="width: 213px;" | 10.2 (8.5–12.5) | |||
| class="left-aligned" style="width: 126px;" | 11 (9.3–13.2) | |||
| class="left-aligned" style="width: 276px;" | Undefined | |||
|- | |||
| class="right-bordered-cell left-aligned" style="width: 80px;" | '''NLR''' | |||
| class="left-aligned" style="width: 213px;" | 0.1 (0.0–0.2) | |||
| class="left-aligned" style="width: 126px;" | Undefined | |||
| class="left-aligned" style="width: 276px;" | 0.1 (0.1–0.4) | |||
|} | |||
== Référence == | == Référence == | ||
[[File:Pdf.jpeg|link=]] Diagnosing acute aortic syndrome: a Canadian clinical practice guideline CMAJ2020 doi: 10.1503/cmaj.200021 | [[File:Pdf.jpeg|Pdf.jpeg|link=]] [[Media:DAo_canadian_rules.pdf|Diagnosing acute aortic syndrome: a Canadian clinical practice guideline]] CMAJ2020 doi: 10.1503/cmaj.200021 | ||
== Mise à jour : | [[File:Pdf.jpeg|Pdf.jpeg|link=]] The sonographic protocol for the emergent evaluation of aortic dissections (SPEED protocol): A multicenter, prospective, observational study AEM 2023 [https://doi.org/10.1111/acem.14839 https://doi.org/10.1111/acem.14839]<br> | ||
== Mise à jour : Juillet 2024 == | |||
| | ||
| | ||
Dernière version du 31 juillet 2024 à 08:57
Algorithme
Evaluation du risque
SPEED protocol
Utilisation de l'ECMU : Le protocole SPEED combine l'échocardiographie transthoracique et l'échographie de l'aorte abdominale.
Cible :
- dissection aortique de type A de Standford
- épanchement péricardique,
- un flap intimal
- un diamètre de l'aorte initial (AOFT) > 35 mm mesuré d'une paroi interne à l'autre à 20 mm de l'anneau aortique en fin de diastole
- dissection aortique de type B de Standford
- un flap intimal dans l'aorte abdominale
valeur du test
| A-AoD and B-AoD (95% CI) | A-AoD (95% CI) | B-AoD (intimal flap only) (95% CI)</thead> | |
|---|---|---|---|
| Accuracy | 91 (89.3–92.5) | 91.1 (89.4–92.6) | 99.8 (99.3–100) |
| Sensitivity | 93.2 (81.3–98.6) | 100 (83.9–100) | 87 (66.4–97.2) |
| Specificity | 90.9 (89.2–92.5) | 90.9 (89.2–92.5) | 100 (99.7–100) |
| PPV | 26.3 (19.6–33.9) | 15.4 (9.8–22.6) | 100 (83.2–100) |
| NPV | 99.7 (99.2–100) | 100 (99.7–100) | 99.8 (99.3–100) |
| PLR | 10.2 (8.5–12.5) | 11 (9.3–13.2) | Undefined |
| NLR | 0.1 (0.0–0.2) | Undefined | 0.1 (0.1–0.4) |
Référence
![]() Diagnosing acute aortic syndrome: a Canadian clinical practice guideline CMAJ2020 doi: 10.1503/cmaj.200021
Diagnosing acute aortic syndrome: a Canadian clinical practice guideline CMAJ2020 doi: 10.1503/cmaj.200021
![]() The sonographic protocol for the emergent evaluation of aortic dissections (SPEED protocol): A multicenter, prospective, observational study AEM 2023 https://doi.org/10.1111/acem.14839
The sonographic protocol for the emergent evaluation of aortic dissections (SPEED protocol): A multicenter, prospective, observational study AEM 2023 https://doi.org/10.1111/acem.14839
Mise à jour : Juillet 2024